3-4 weeks of consults and testing, or 1 day, if you do our Same Day 360° Evaluation.
We examine your unique case: your medical history, requirements, and results of your testing (antral follicle count, evaluation of your uterus and ovaries, and hormonal evaluation). Then we’ll choose from over fifteen treatment protocols to find the best fit for you.
We have several goals as we move through your plan:
Together we’ll discuss each step and all your options. We’ll give our recommendations and help you determine which approach is best for you.
Spring Fertility offers a Comprehensive Same Day 360° Evaluation of both partners. In just four hours, you’ll know your options and have a plan.
This phase lasts about 8–12 days per cycle and is the most time-intensive.
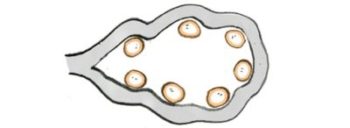
36 hours later, we retrieve your eggs through a 20 minute procedure.
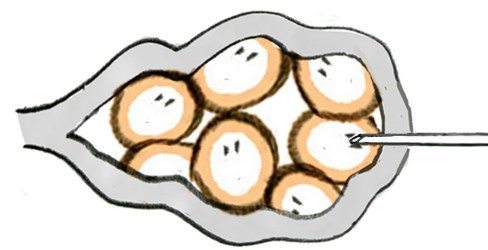
You’ll check in about an hour before the procedure, to prep and change into a warm robe before meeting our anesthesiologist and embryologist who will be caring for you and your eggs. You’ll fall asleep under anesthesia, while our specialists aspirate your eggs using a very fine needle.
About 20 minutes later, you’ll awaken in our recovery area where our team will look after you before you are ready to go home (usually about 45 minutes). Most people take the rest of the day off and are ready to go back to work the next day.
Same day as the egg retrieval, either during the procedure or shortly thereafter.
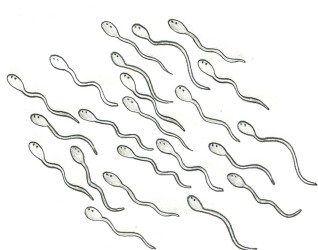
The most common way sperm is collected is by ejaculation of a sample, usually on the day of the egg retrieval within a private production room here at Spring Fertility. Some patients elect to collect the specimen at home, for drop off within two hours of ejaculation.
Prior to IVF or ICSI, the sperm is carefully processed in our Andrology lab by our expert embryologists. In a process that takes about 1-2 hours, the healthiest and most motile sperm are separated and washed to remove bacteria and other unwanted components. The sperm cells are activated and a particular density – or concentration – of the best sperm is achieved. This way, we find the best swimmers to optimize fertilization.
4-6 hours after the egg retrieval.
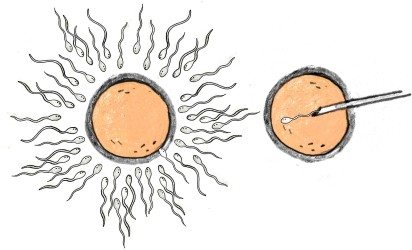
Now that we have eggs and sperm, it’s time for them to meet (insemination). This can be done in one of two ways: conventional insemination (IVF) or through ICSI. Both procedures are performed outside the body by our team of expert specialists.
IVF (In Vitro Fertilization)
ICSI (Intra-cytoplasmic Sperm Injection)
In a 2013 report from the CDC, 69% of IVF cycles in the United States used ICSI.
*Split ICSI: In couples with unexplained infertility, about 1 in 12 will experience poor fertilization when using conventional insemination (despite a normal appearing semen analysis). For this reason, your physician may suggest performing ICSI on half of your eggs. This helps us identify if fertilization has been the primary obstacle preventing you from getting pregnant. It also saves half the cycle if the eggs do not fertilize well with conventional insemination, because ICSI can be effective for the other eggs. Some people choose to use ICSI on all the eggs in order to minimize their risk.
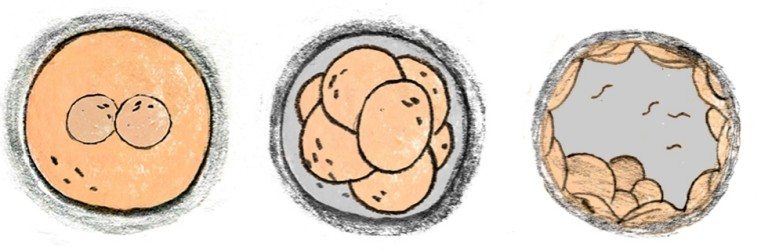
Fertilization Check
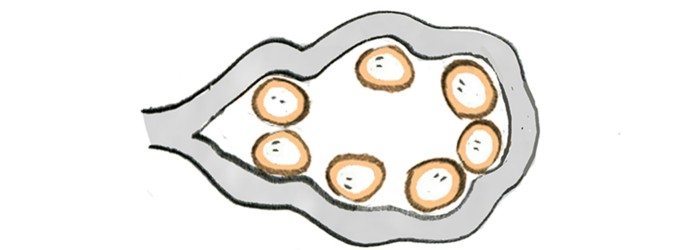
The morning after insemination, we check to see if the eggs fertilized. Normally fertilized eggs have two “pronuclei,” DNA from the sperm and from the egg. Your fertilized egg is officially called an embryo.
Days in Lab: Day 2-3 Embryos vs Day 5-6 Embryos (a “Blastocyst”)
Today, we increasingly care for embryos in the lab for 5–6 days until they reach the blastocyst stage. This gives us time to determine which are healthiest to be transferred back to the uterus. Patients with fewer good quality embryos may choose to transfer the embryo back into the uterus 2 or 3 days after fertilization since we are not choosing between them.
To Test or Transfer?
IVF patients now have the opportunity to test their embryos before transferring them. This process, called Preimplantation Genetic Testing, allows us to maximize the likelihood of success by carefully sampling a few cells from each embryo and testing them to see if they are chromosomally normal (PGS-screening). We can also test embryos to diagnose a disease that one or both parents are known to carry (PGD-diagnosis). This test also tells us the gender of your embryo, but we can keep that a secret if you prefer. While those cells are being analyzed, your embryos are safely cryopreserved with us. Cryopreservation of embryos has been safely performed for over 30 years, and today over 99% of embryos survive with no negative effects on IVF outcomes. To learn more, see our FAQ.
The big day, timed to your unique case and plan.
Fresh Or Frozen
Some patients choose to transfer embryos fresh (a few days after retrieval). Others freeze their embryos and transfer them later. Patients pursuing preimplantation genetic testing will need to freeze their embryos while we await the test results.
In recent years, frozen embryo transfers have become increasingly popular as the success and outcomes have proven at least as good as fresh transfers. We believe this decision can be individualized based on your history and response to the medications. Occasionally, we will recommend embryo cryopreservation and a frozen transfer during the cycle, depending on how your body and the embryos develop. For more on this decision, please see our FAQ.
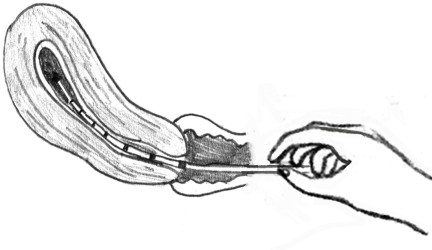
The Transfer Procedure
We double confirm that we’ve got your best embryo(s). You’ll arrive early to change and get ready. There’s no anesthesia required, but we recommend Valium to minimize uterine contractions. You’ll watch us on a closed circuit television as we gently draw your embryo into a thin soft catheter for transfer. You’ll then watch by ultrasound as the embryos are returned to your uterus.
The transfer itself takes a few minutes and is not painful. The primary discomfort you may experience is from a full bladder we ask you to have so that we can all see best by ultrasound.
About 2 weeks after the transfer, fresh or frozen.
You’ll come back 11–13 days after the transfer to find out if the embryos implanted successfully. We know waiting can be the hardest part—and we’re with you every step of the way. We’ve partnered with local wellness providers to help you stay positive and healthy while your embryo(s) should be implanting.